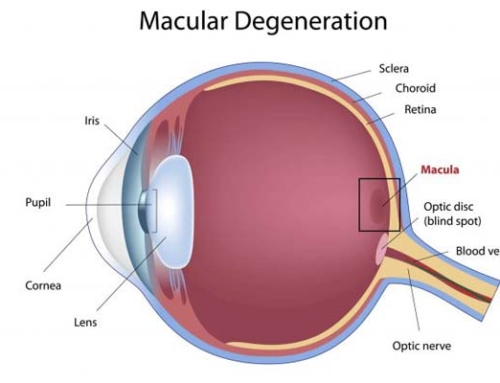
Keratoconus is an eye disease that can occur in one or both of the eyes, and it usually starts during the teenage years. The cornea which is normally round, progressively starts to bulge and look like a cone. Because of this, the light is deflected on its way to the retina, and is causing a distorted vision.
Keratoconus Symptoms
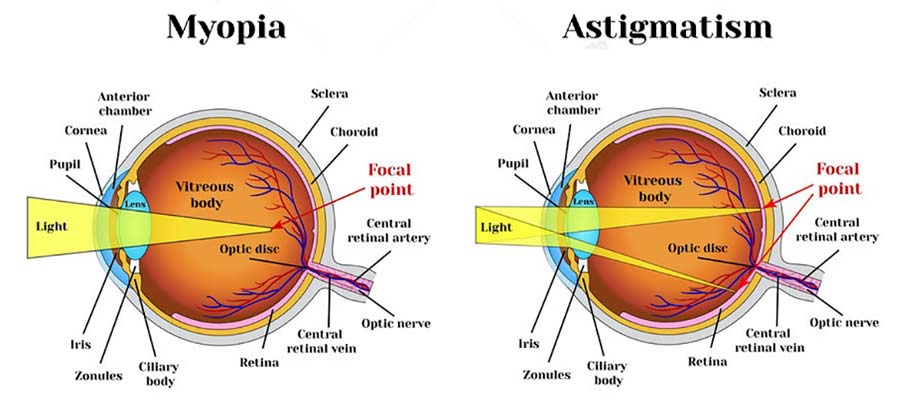
What initially appears as a myopia (nearsightedness) or astigmatism, then evolves. The patient needs a new prescription for eyeglasses each time they visit the doctor, since the cornea is constantly changing its shape. Symptoms include:
- Distorted vision
- Blurred vision
- Glare
- Light sensitivity
Causes of Keratoconus
The latest research is showing that this eye condition occurs because of an imbalance of the enzymes inside the cornea. This allows the cornea to be affected by free radicals (oxidative damage), become weaker and then bulge forward. Causes may include:
- A genetic predisposition (usually if parents have this condition it is most likely to be transmitted to kids)
- Too much exposure to UV rays from the sun
- Rubbing the eyes too much
- Wearing misfit contact lenses
- A chronic irritation of the eye
Keratoconus Treatment
Initially this condition can be corrected with prescription glasses or soft contact lenses. But as it progresses and the cornea becomes more irregular, these measures won’t help anymore. There are other methods that can cure keratoconus, they are as follows:
- Corneal crosslinking
This method is also known as CXL and it implies strengthening the corneal tissue in order to stop it from changing its shape. This procedure has 2 possible options: the epithelium-off and the epithelium-on. When the epithelium-off crosslinking is made, the outer layer of the cornea is removed in order to allow riboflavin to enter. This is then activated with UV light and it strengthens the cornea. During the other method (epithelium-on), the tissue is left intact. While it does take more time for the riboflavin to enter the cornea, it also has fewer side effects (such as an infection or discomfort). The recovery of the sight also takes place much faster. These methods are efficient in most cases and reduce the need for corneal transplants. They are also used in order to prevent or to treat complications after corrective surgeries such as LASIK. Sometimes they are also combined with other methods in order to offer the best results.
- Custom soft contact lenses
This kind of lens has been recently introduced and it can correct mild or moderate forms of keratoconus. Since this condition is unique to each and every person, these lenses are custom made for each one of them. This means that they are more comfortable as well. There are various types of such lenses made by different companies, and they can correct up to 30 diopters of myopia or hyperopia, and up to -12 diopters of astigmatism.
- Gas permeable contact lenses
If the previous methods don’t work, then this one is preferred. These lenses cover the irregular shape of the cornea with a smooth and uniform surface that is also refractive. This method is time consuming and you might need to do multiple visits to your doctor in order to fine tune the lenses until they offer perfect vision. As the keratoconus progresses and the cornea changes its shape again, more tuning will be needed.
- “Piggybacking” contact lenses
The previous methods can be uncomfortable for some patients, so many practitioners prefer this one. It involves the process of “piggybacking” the two types of lenses mentioned before on the same eye. Usually a soft contact lens is added on the eye surface, and then a gas permeable lens is added on top of it. This process needs to be supervised by your doctor in order to make sure that enough oxygen reaches the eye surface.
- Hybrid contact lenses
These lenses are also a combination of the two types mentioned above. They offer the clear optics of a gas permeable contact lens combined with the comfort of wearing a soft lens. They are available in various shapes and sizes in order to adapt with the irregular eye affected by keratoconus.
- Scleral and semi scleral lenses
Their name comes from the fact that they are much larger than the gas permeable lenses, covering a part of the white of the eye (the sclera). Scleral lenses are larger, while semi scleral ones only cover a small part. Thanks to their shape they don’t apply any pressure to the eye, so they are more comfortable. They are also more stable, compared to other types which move with each blink of the eye.
- Prosthetic lenses
Because of some cases of keratoconus are very severe, none of the methods above doesn’t work. In this case a prosthetic lens may be the right solution. For severe or untreatable eyes, prosthetic lenses have worked very well since the 1990’s, restoring eye sight, reducing the symptoms and improving the quality of life. Since then various companies are making their own prosthetic lenses, each with its own benefits.
- Intacs
When glasses no longer provide a clear vision, intacs are needed. These are corneal inserts with the shape of an arc that are surgically placed on the cornea to reshape its surface. The entire procedure takes only 10 minutes, and these implants are also removable and can be changed. They can’t prevent a corneal transplant if the condition is still progressing, but they can delay it for a few years.
- Topography guided conductive keratoplasty
Simply known as CK, this procedure helps to smooth the irregularities on the surface of the cornea. A topographic map of the eye is first created, and then radio waves are used to reshape it.
- Corneal transplant
If all the previous methods don’t work anymore or if the person simply can’t stand to wear a lens, then a corneal transplant may be the only solution left. It is also known as penetrating keratoplasty (PK) and it does not guarantee a perfect vision. Even after the transplant, some patients may still need to wear glasses or lenses. If you suffer from keratoconus or feel like your vision could be better, please follow up with your eye doctor to discuss your treatment options. Thank you for reading.